Medical Billing: Why Didn't My Bill Get Shared?
%20(900%20x%20900%20px)%20(950%20x%20700%20px)%20(8).webp?width=950&height=700&name=blogImages%20-%20Impact%20(1200%20x%20630%20px)%20(900%20x%20900%20px)%20(950%20x%20700%20px)%20(8).webp)
Key Highlights
- The Importance of Medical Billing: Medical billing is crucial for healthcare providers to receive accurate compensation for their services, ensuring the financial stability of the healthcare system.
- A Complex Process: It involves a detailed series of steps, from patient registration and insurance verification to coding, charge entry, claim submission, and follow-ups.
- Understanding Your Insurance: Patients must understand their insurance coverage, including benefits, copayments, deductibles, and out-of-network implications, to anticipate potential costs. For Impact members this means understanding your healthcare sharing organization and the guidelines of sharing.
- Preventing Billing Errors: Providing accurate patient information and keeping medical records up-to-date are essential to minimize billing errors.
- Addressing Billing Issues: If discrepancies arise, contact your healthcare provider and healthcare company to understand the nature of the issue and seek resolution.
Introduction
In the United States, the medical billing process is very important. It helps healthcare providers get paid fairly for their work. This process involves sharing information between patients, healthcare providers, and health care companies. Each group has its own financial responsibilities. But sometimes, the process can be tricky. Many factors can cause billing problems. This can lead to confusion and frustration for patients.
Understanding Medical Billing in the United States
Healthcare providers bill insurance or healthcare sharing companies and sometimes patients directly for the medical services they provide. Medical billing helps these groups work together by sharing important information and payments.
This system is complex and requires special knowledge of medical codes, such as ICD, CPT, and HCPCS. These codes help represent procedures and diagnoses to get paid back. It also requires following strict rules, like HIPAA, which shows why trained professionals are needed in this area.
The Role of Medical Billers in Healthcare
Medical billers are very important in the healthcare revenue cycle. They collect patient details and healthcare information, check for errors and with healthcare sharing, check the guidelines, and make sure the coding of medical procedures and diagnoses is correct. Their careful work turns patient visits into bills that can be easily read.
Medical billers act as a link between healthcare providers and healthcare companies like Impact Health Sharing. They send bills and keep a close eye on their status. If any bill is denied or rejected, they look into why it happened. They take action, like appealing decisions or fixing coding mistakes.
In addition, medical billers help improve the revenue cycle management for healthcare providers. They reduce denials, speed up the reimbursement process, and ensure accurate billing. This greatly supports the financial health of healthcare organizations.
How to Address and Prevent Billing Errors
Addressing billing errors needs a proactive approach. If you see any mistakes on your medical bill, contact your healthcare provider's billing department right away. They can check the charges and clear up any confusion.
At the same time, reach out to Impact to confirm that your services will be shared or applied to your PRA. Remember, good communication and quick action can fix most billing issues easily.
Importance of Accurate Patient Data
One of the best ways to stop billing mistakes is to make sure your personal and healthcare details are correct. When you register, check all the information you put in. If anything changes, like your address or contact details, tell your provider right away.
Correct patient information is key for a smooth billing process. It affects both how happy patients are and how well healthcare providers do financially. Keeping your patient’s medical history and medical records up-to-date is just as important. Let your providers know about any pre-existing conditions, allergies, medications, or past treatments so they can build a full medical history for you.
By helping keep your medical records accurate, you lower the chance of billing issues. This also avoids delays in treatment and makes sure you get billed correctly for the services you receive.
Regular Audits and Compliance Checks
Healthcare providers and professional billing departments need to make regular audits and compliance checks a priority. This helps keep billing practices accurate and ethical in the healthcare industry. Audits involve carefully reviewing medical records, billing codes, and claims. This way, they can spot and fix errors or mismatches.
Regular audits and compliance checks aren't just routine tasks; they show a dedication to ethical billing, accurate financial records, and building patient trust. Using these practices helps protect the billing process and creates a sense of responsibility in the healthcare industry.
Navigating Through Healthcare Guidelines
Understanding your insurance policy is important. It helps you avoid surprises when you get your medical bill. You should know your plan's coverage limits, deductibles, copayments, and benefits for out-of-network services.
Always keep a copy of your insurance card close. Tell your healthcare provider if there are any changes to your policy. If a claim is denied, get in touch with your insurance company. Ask them why the claim was denied and look for ways to appeal.
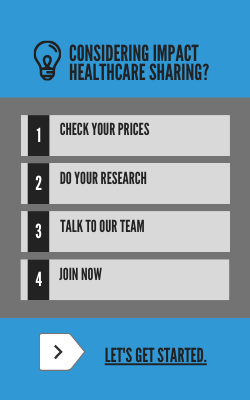
Understanding Sharing Eligibility
Navigating the Impact Member Guidelines will take some time. Start by learning the basics. This includes what is shared and what is not, PRA, provider fee amounts, and perks that won't cost you a thing like wellness labs and Telehealth.
The Billing Process
When a healthcare provider sends a bill to Impact, this starts the process of repricing where we take a closer look at the billing details. Reference Based Repricing ensures fair and just pricing for all claims. Our approach includes three key components to ensure claims are priced fairly for everyone involved. First, we audit each claim using our industry-leading Medical Bill Review program. This helps us identify any inaccuracies or inconsistencies in the billing process. Next, we determine the "best price" for each claim using multiple methodologies and 15 years of claims history. This includes utilizing historical data, reference-based benchmarks, direct contracts, fair market value, and fee-for-service pricing. Finally, we determine what is considered fair-marketing pricing for the services rendered.
If this is a shareable need, then it will be shared among members if the PRA has already been met. If the PRA has not been met, then the amount will be applied, and you will be responsible for paying that amount.
Common Reasons for Billing Issues
Even with a careful process, billing problems can happen. These issues often come from small mistakes. For example, there could be typos in patient information, wrong healthcare program details, or missing bill information for certain procedures.
Also, mistakes in coding or differences between what services were provided and the patient's healthcare program can cause claims to be denied. This makes the billing process harder. It is important for healthcare providers and patients to know these possible problems to make things easier.
Medical Program Verification Failures
One key reason medical bills aren't shared quickly is due to problems with program verification. It is very important to check a patient's healthcare program with their provider before any medical service.
This check makes sure the patient is active. It also confirms the benefits they have and any provider fees and personal responsibility amount they need to meet. If this step is skipped or if there is incorrect information, it can lead to denied bills. This leaves patients and providers to deal with surprise costs.
Poor verification not only slows down billing but also affects the patient’s financial planning. It may make them hesitant to seek needed medical care because they are unsure about what is shared. Because of this, paying close attention to detail is crucial for smooth medical billing.
Incorrect Patient Information
Imagine this situation: you go to your doctor and get treatment, but you never receive a bill. When you check, you find that a small mistake made during patient registration, like a wrong name or date of birth, has turned into a big billing problem.
This shows how important accurate data entry is in healthcare. Mistakes in recording or updating patient information, such as addresses, contact details, and insurance information, can cause confusion and lead to slow or misdelivered bills.
It's very important to show your member card at each provider's office so they can enter the details into their billing system.
The Role of Medical Billers in Healthcare
Medical billers are very important in the healthcare revenue cycle. They collect patient details and healthcare information, check for coverage or with healthcare sharing, check the guidelines, and make sure the coding of medical procedures and diagnoses is correct. Their careful work turns patient visits into bills that can be easily read.
Medical billers act as a link between healthcare providers and healthcare companies like Impact Health Sharing. They send bills and keep a close eye on their status. If any bill is denied or rejected, they look into why it happened. They take action, like appealing decisions or fixing coding mistakes.
In addition, medical billers help improve the revenue cycle management for healthcare providers. They reduce denials, speed up the reimbursement process, and ensure accurate billing. This greatly supports the financial health of healthcare organizations.
Key Components of a Medical Bill
A medical bill can seem confusing at first. However, if you learn about its main parts, it gets easier to understand the charges.
One important part is the Current Procedural Terminology (CPT) codes developed by the American Medical Association (AMA). These codes use numbers to show every medical, surgical, and diagnostic procedure done during a patient visit.
Another part is the International Classification of Diseases ICD codes. These codes describe the patient's health condition in a standard way. This helps with accurate billing and data analysis.
There's also the Healthcare Common Procedure Coding System (HCPCS). This system is used to note extra services or equipment. This includes things like durable medical equipment, ambulance services, or specific medications. Using these codes correctly helps healthcare providers get paid properly for their services.
%20(900%20x%20900%20px)%20(950%20x%20700%20px)%20(6).webp?width=950&height=700&name=blogImages%20-%20Impact%20(1200%20x%20630%20px)%20(900%20x%20900%20px)%20(950%20x%20700%20px)%20(6).webp)
Even with a careful process, billing problems can happen. These issues often come from small mistakes. For example, there could be typos in patient information, wrong healthcare program details, or missing bill information for certain procedures.
Also, mistakes in coding or differences between what services were provided and the patient's healthcare program can cause claims to be denied. This makes the billing process harder. It is important for healthcare providers and patients to know these possible problems to make things easier.
Medical Program Verification Failures
One key reason medical bills aren't shared quickly is due to problems with program verification. It is very important to check a patient's healthcare program with their provider before any medical service.
This check makes sure the patient is active. It also confirms the benefits they have and any provider fees and personal responsibility amount they need to meet. If this step is skipped or if there is incorrect information, it can lead to denied bills. This leaves patients and providers to deal with surprise costs.
Poor verification not only slows down billing but also affects the patient’s financial planning. It may make them hesitant to seek needed medical care because they are unsure about what is shared. Because of this, paying close attention to detail is crucial for smooth medical billing.
Incorrect Patient Information
Imagine this situation: you go to your doctor and get treatment, but you never receive a bill. When you check, you find that a small mistake made during patient registration, like a wrong name or date of birth, has turned into a big billing problem.
This shows how important accurate data entry is in healthcare. Mistakes in recording or updating patient information, such as addresses, contact details, and insurance information or healthcare sharing information, can cause confusion and lead to slow or misdelivered bills.
It's very important to show your member card at each provider's office so they can enter the details into their billing system.
The Medical Billing Process Explained
The medical billing process has several steps, including the adoption of medical billing software. These steps aim to ensure things are accurate, clear, and effective in dealing with money in our healthcare system. Knowing this process can help both healthcare providers and patients manage the difficult parts of billing.
It all starts with patient registration. After that, healthcare verification occurs. Here, sharing details and benefits are checked. Then, medical coding takes place, which means turning medical procedures and procedure codes into specific codes. These codes are important because they are used to create and send claims to insurance companies for payment or bills to healthcare sharing organizations.
Patient Registration and Verification
The medical billing process starts with patient registration. This usually happens during the first visit or when joining a healthcare facility. In this step, important information is gathered. This includes the patient's name, date of birth, address, contact details, and healthcare information, all contributing to patient satisfaction.
After the patient registration is done, the next key step is verification. It helps to make sure that the healthcare provider will get paid for the services given. This step involves reaching out to the patient's healthcare company to confirm details. This includes effective dates and details about the health program they are enrolled in.
From Service Delivery to Bill Submission
After medical services are provided, the billing process begins. The healthcare provider carefully writes down the procedures done, the diagnoses made, and any treatments given.
Trained medical coders then change this information into standard medical codes, like CPT, ICD, and HCPCS. These codes help healthcare providers and companies speak the same language, which makes communication clear about the health care services given.
After coding is done, electronic claims are created and sent to Impact. Submitting these bills well, with no mistakes, is very important for getting paid on time.
%20(900%20x%20900%20px)%20(950%20x%20700%20px)%20(7).webp?width=950&height=700&name=blogImages%20-%20Impact%20(1200%20x%20630%20px)%20(900%20x%20900%20px)%20(950%20x%20700%20px)%20(7).webp)
Conclusion
In conclusion, having correct and clear patient health information is very important. Regular checks also help prevent mistakes in medical billing. When patients are aware of and take steps to understand the guidelines and what type of services are eligible for sharing, they can avoid billing problems. It is crucial to take control of your healthcare costs. This way, you can address and challenge any issues that show up.
Frequently Asked Questions
What to Do If Your Medical Bill Wasn't Shared?
If you did not get a medical bill, start by calling your healthcare provider. Make sure they have your healthcare information and address. Impact processes bills in the order in which they are received. You can see the status of your medical bill in the ShareStream in your Member Center. Click the bill number to view more details about your bill.
What if my doctor will not accept Impact?
Although this is rare, it is possible. If a provider has questions, it's best to call the toll-free number on the back of the member ID card and follow the provider-specific prompts. The Impact specialist will explain the program in further detail and negotiate if necessary. If they don't want to call, you can read more directions here.
How to Dispute a Billing Error?
Impact evaluates each sharing request under these Guidelines. At times, the validity of a Member’s request may be unclear. In these situations, Impact must then exercise discretionary judgment on behalf of the entire Impact membership to evaluate the request, using common sense and fairness as a guide. Medical records may also be required to aid in determining if sharing is eligible. See the detailed instructions here.

%20(900%20x%20900%20px)%20(950%20x%20700%20px)%20(5)-1.webp?width=300&name=blogImages%20-%20Impact%20(1200%20x%20630%20px)%20(900%20x%20900%20px)%20(950%20x%20700%20px)%20(5)-1.webp)